Soap Objective . soap notes include a statement about relevant client behaviors or status (subjective), observable, quantifiable, and. soap notes are a specific format for writing progress notes as a behavioral health clinician. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. learn how to write a soap note so you can efficiently track, assess, diagnose, and treat clients. They contain four primary sections, represented by its acronym: soap notes are a structured way of recording the progress of a patient during treatment by health professionals. here’s how to write the objective in soap notes, what information to include, and examples of what to put in the objective. documenting a patient assessment in the notes is something all medical students need to practice.
from www.slideserve.com
They contain four primary sections, represented by its acronym: soap notes are a specific format for writing progress notes as a behavioral health clinician. soap notes include a statement about relevant client behaviors or status (subjective), observable, quantifiable, and. learn how to write a soap note so you can efficiently track, assess, diagnose, and treat clients. documenting a patient assessment in the notes is something all medical students need to practice. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. here’s how to write the objective in soap notes, what information to include, and examples of what to put in the objective. soap notes are a structured way of recording the progress of a patient during treatment by health professionals.
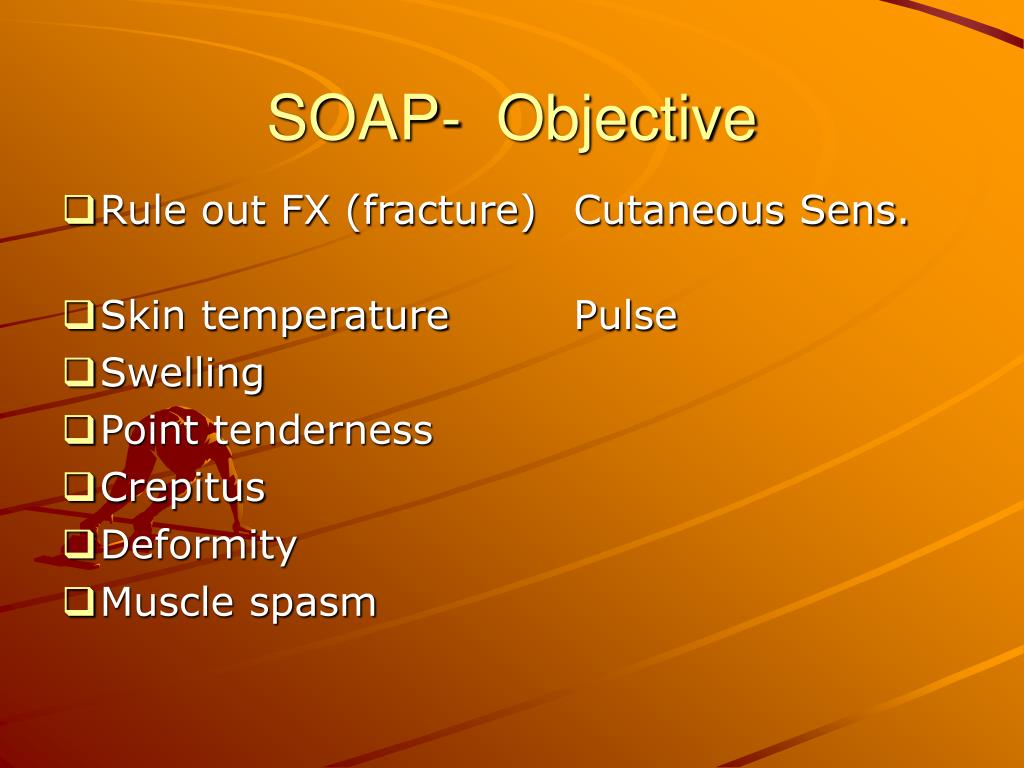
PPT Injury Evaluation Basics PowerPoint Presentation, free download ID983764
Soap Objective soap notes are a structured way of recording the progress of a patient during treatment by health professionals. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. They contain four primary sections, represented by its acronym: documenting a patient assessment in the notes is something all medical students need to practice. soap notes are a structured way of recording the progress of a patient during treatment by health professionals. learn how to write a soap note so you can efficiently track, assess, diagnose, and treat clients. soap notes are a specific format for writing progress notes as a behavioral health clinician. soap notes include a statement about relevant client behaviors or status (subjective), observable, quantifiable, and. here’s how to write the objective in soap notes, what information to include, and examples of what to put in the objective.
From www.examples.com
SOAP Note 19+ Examples, Format, How to Write, PDF Soap Objective soap notes include a statement about relevant client behaviors or status (subjective), observable, quantifiable, and. soap notes are a structured way of recording the progress of a patient during treatment by health professionals. soap notes are a specific format for writing progress notes as a behavioral health clinician. here’s how to write the objective in soap. Soap Objective.
From ceewdssy.blob.core.windows.net
Soap Note Objective at Jannie Munos blog Soap Objective They contain four primary sections, represented by its acronym: documenting a patient assessment in the notes is something all medical students need to practice. here’s how to write the objective in soap notes, what information to include, and examples of what to put in the objective. the subjective, objective, assessment and plan (soap) note is an acronym. Soap Objective.
From www.slideserve.com
PPT SOAP Notes PowerPoint Presentation, free download ID1111245 Soap Objective here’s how to write the objective in soap notes, what information to include, and examples of what to put in the objective. soap notes are a specific format for writing progress notes as a behavioral health clinician. They contain four primary sections, represented by its acronym: documenting a patient assessment in the notes is something all medical. Soap Objective.
From www.slideserve.com
PPT Sports Injury Assessment PowerPoint Presentation, free download ID6694393 Soap Objective soap notes are a structured way of recording the progress of a patient during treatment by health professionals. here’s how to write the objective in soap notes, what information to include, and examples of what to put in the objective. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of.. Soap Objective.
From www.pinterest.com
Soap Report Template in 2023 Soap note, Notes template, Nurse study notes Soap Objective the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. documenting a patient assessment in the notes is something all medical students need to practice. They contain four primary sections, represented by its acronym: soap notes include a statement about relevant client behaviors or status (subjective), observable, quantifiable, and. . Soap Objective.
From www.studocu.com
Hospital Dentistry SOAP (Subjective, Objective, Plan, Assessment) DENTISTRY I LEC [SOAP Soap Objective soap notes are a specific format for writing progress notes as a behavioral health clinician. soap notes are a structured way of recording the progress of a patient during treatment by health professionals. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. learn how to write a soap. Soap Objective.
From exoeqjxxj.blob.core.windows.net
Soap Note Objective Findings at Sherry Miller blog Soap Objective the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. They contain four primary sections, represented by its acronym: soap notes are a specific format for writing progress notes as a behavioral health clinician. documenting a patient assessment in the notes is something all medical students need to practice. . Soap Objective.
From doctemplates.us
Soap Note Objective Example DocTemplates Soap Objective soap notes include a statement about relevant client behaviors or status (subjective), observable, quantifiable, and. They contain four primary sections, represented by its acronym: the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. documenting a patient assessment in the notes is something all medical students need to practice. . Soap Objective.
From exoeqjxxj.blob.core.windows.net
Soap Note Objective Findings at Sherry Miller blog Soap Objective here’s how to write the objective in soap notes, what information to include, and examples of what to put in the objective. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. soap notes include a statement about relevant client behaviors or status (subjective), observable, quantifiable, and. learn how. Soap Objective.
From cemrcbfw.blob.core.windows.net
Soap Making Objectives at Stephen Bierman blog Soap Objective learn how to write a soap note so you can efficiently track, assess, diagnose, and treat clients. soap notes include a statement about relevant client behaviors or status (subjective), observable, quantifiable, and. soap notes are a specific format for writing progress notes as a behavioral health clinician. soap notes are a structured way of recording the. Soap Objective.
From exoeqjxxj.blob.core.windows.net
Soap Note Objective Findings at Sherry Miller blog Soap Objective here’s how to write the objective in soap notes, what information to include, and examples of what to put in the objective. soap notes are a structured way of recording the progress of a patient during treatment by health professionals. soap notes include a statement about relevant client behaviors or status (subjective), observable, quantifiable, and. documenting. Soap Objective.
From slidetodoc.com
Documentation SOAP Notes Documenting Injury Evaluation Information documentation Soap Objective soap notes are a specific format for writing progress notes as a behavioral health clinician. They contain four primary sections, represented by its acronym: soap notes are a structured way of recording the progress of a patient during treatment by health professionals. here’s how to write the objective in soap notes, what information to include, and examples. Soap Objective.
From exoeqjxxj.blob.core.windows.net
Soap Note Objective Findings at Sherry Miller blog Soap Objective soap notes are a structured way of recording the progress of a patient during treatment by health professionals. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. documenting a patient assessment in the notes is something all medical students need to practice. soap notes are a specific format. Soap Objective.
From www.studocu.com
SOAP Note Example S.O.A. Note Template CASE ID ____________________________ Subjective Soap Objective soap notes are a structured way of recording the progress of a patient during treatment by health professionals. here’s how to write the objective in soap notes, what information to include, and examples of what to put in the objective. soap notes include a statement about relevant client behaviors or status (subjective), observable, quantifiable, and. soap. Soap Objective.
From www.slideserve.com
PPT Injury Evaluation Basics PowerPoint Presentation, free download ID983764 Soap Objective soap notes are a structured way of recording the progress of a patient during treatment by health professionals. soap notes are a specific format for writing progress notes as a behavioral health clinician. soap notes include a statement about relevant client behaviors or status (subjective), observable, quantifiable, and. the subjective, objective, assessment and plan (soap) note. Soap Objective.
From exoeqjxxj.blob.core.windows.net
Soap Note Objective Findings at Sherry Miller blog Soap Objective They contain four primary sections, represented by its acronym: the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of. soap notes are a specific format for writing progress notes as a behavioral health clinician. soap notes are a structured way of recording the progress of a patient during treatment by. Soap Objective.
From www.sampletemplates.com
FREE 9+ Sample Subjective Objective Assessment Planning Notes in PDF MS Word Soap Objective here’s how to write the objective in soap notes, what information to include, and examples of what to put in the objective. soap notes include a statement about relevant client behaviors or status (subjective), observable, quantifiable, and. documenting a patient assessment in the notes is something all medical students need to practice. soap notes are a. Soap Objective.
From cemrcbfw.blob.core.windows.net
Soap Making Objectives at Stephen Bierman blog Soap Objective soap notes are a structured way of recording the progress of a patient during treatment by health professionals. soap notes are a specific format for writing progress notes as a behavioral health clinician. documenting a patient assessment in the notes is something all medical students need to practice. learn how to write a soap note so. Soap Objective.